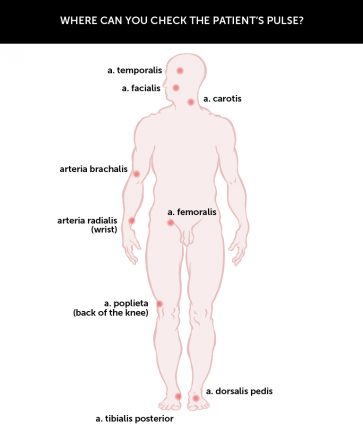
Pulse rate is an important observation when assessing the patient’s circulation. The nurse should count the pulse frequency, regularity and pulse character. Normal pulse rate is approximately 65-80 beats per minute and is steady and regular. Pulse rate over 100 beats per minute is called tachycardia and a pulse rate below 60 beats per minute is called bradycardia. Because of varying preload in the left ventricle, the heartbeats may be different in strength. In cardiac arrhythmias such as atrial fibrillation patients may have an irregular pulse. A weak pulse may indicate a reduced stroke volume and ejection fraction (percentage of left ventricular end-diastolic volume) and increased systemic resistance (vasoconstriction). It is therefore important that the pulse is counted manually and not only by means of a monitoring device. The pulse should be counted for a full minute. The radial pulse can be palpated at the wrist and is the most common site to record pulse rate. If however the the systolic blood pressure (BP) is <80 mm Hg, if the patient is in shock, or if there are presenting symptoms indicating that the patient has suffered a cardiac arrest the pulse should be palpated in other arteries namely the brachial artery, the femoral artery or the carotid artery.
| Diagnosis | Systolic bloodpressure (mm Hg) | Diastolic bloodpressure (mm Hg) |
|---|---|---|
| Optimal BP | <120 | <80 |
| Normal BP | <130 | <85 |
| High normal BP | 130-139 | 85-89 |
| Grade 1 hypertension (mild) | 140-159 | 90-99 |
| Grade 2 hypertension (moderate) | 160-179 | 100-109 |
| Grade 3 hypertension (serious) | >180 | >110 |
| Isolated systolic hypertension | >140 | <90 |
| Source: Table from 'Helsedirektoratet Retningslinjer for forebygging av hjerte- og karsykdommer 2009' (pdf). Definitions and classifications of blood pressure are in relation to repeated measurements of office blood pressure. (Source: 51. Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003 Nov; 21:1983-92. 52. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, et al. European Guidelines on cardiovascular disease prevention in clinical practice: third joint task force of European and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of eight societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2003;10: S1-S10. 53. ESH/ESC Guidelines Committee. Guidelines for the management of arterial hypertension. Eur Heart J. 2007;28: 1462-536.) | ||
The pulse is affected by the following factors: age, gender, activity, hormones, pain, anxiety, temperature, blood pressure, nausea and physical exercise. The pulse rate is regulated partly by the sympathetic and parasympathetic nervous system, hormonal and electrolyte balance, concentration of oxygen and carbon dioxide in the blood and possibly content of drugs or toxic substances (Jakobsen et al. 2010).
Blood pressure (BP) is defined as the pressure exerted against the blood vessel wall and it is not uniform throughout the cardiac cycle. The distance from the heart, the size of the blood vessels and resistance in vessel walls affects blood pressure. Blood pressure decreases on the way out of the left ventricle and out to the body and is at its highest in the arteries, falls sharply in the capillaries and is almost zero in the large veins. Arterial, capillary pressure and venous pressure refers to pressure in the vascular system. Normally blood pressure in adults is defined as less than 130/85 mm Hg and if blood pressure is 140/90 mm Hg or higher, it is classified as hypertension (NICE, 2011).
Several physical factors affect the arterial blood pressure (Sand et al. 2006) including cardiac output, peripheral resistance, arterial elasticity, blood volume (Eikeland MCA. in Almås 2010, p. 210). Arterial blood pressure increases with age, but a blood pressure higher than 140/90 mm Hg is unfavourable in all circumstances due to cardiac stress (Jakobsen et al. 2010). Systemic blood pressure is recorded indirectly (non-invasively) using a blood pressure device, while direct blood pressure (invasive) is measured directly in the bloodstream by means of an arterial tap.
The skin should be observed to assess for changes in circulation. The nurse should observe skin temperature (whether it’s dry / damp, cold / hot), presence of cyanosis (bluish pallor and colour) on the lips, around the mouth, oral mucosa, conjunctiva, ear lobes and nail beds. In patients with dark skin the pallor of the skin may be seen as ash or more yellowish brown, depending on the colour initially. In patients experiencing shock the skin becomes cold and clammy due to reduced renal blood flow.
Peripheral circulation is assessed by observing the patient’s arms and feet, where comparing skin temperature, symmetry, oedema, pigmentation, ulceration and scarring. By pressing a fingertip against the patient’s nail bed the nurse can examine capillary refill. This should normally occur immediately, but in a patient with reduced peripheral circulation it may be more than 2 seconds.
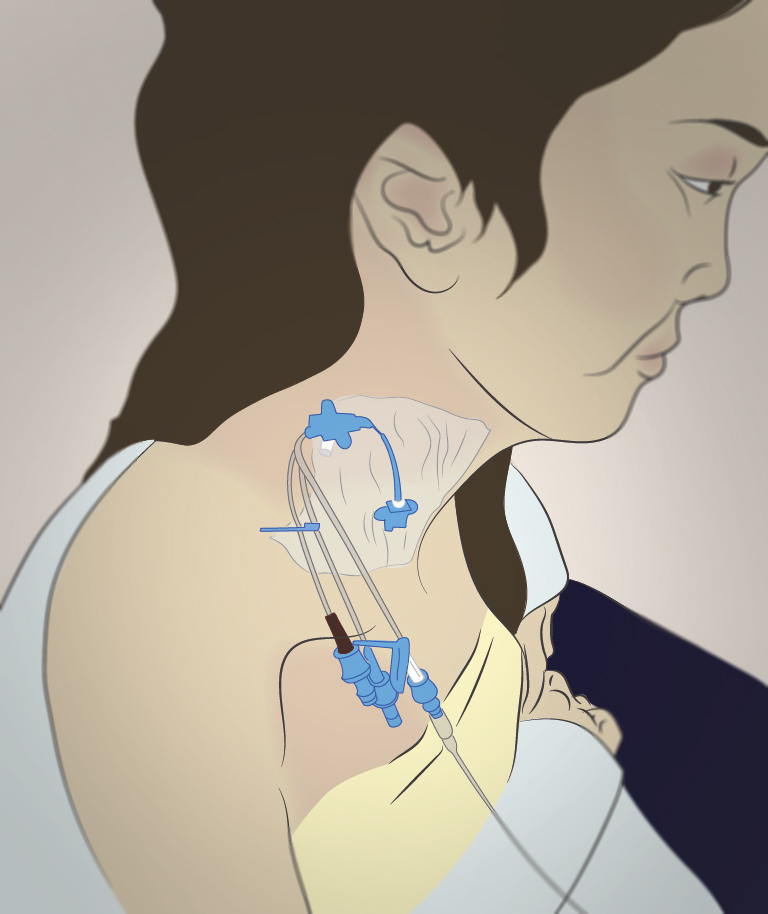
Central venous pressure (CVP) represents the pressure in the vena cava near the entrance to the right atrium, and is an expression of the right ventricular end-diastolic filling pressure. CVP provides an indication of intravascular volume (volume in the bloodstream) and is commonly used to control intravenous fluid therapy. CVP in an adult is from 4 to 10 mm Hg (8-12 cm H2O). Low CVP suggests that circulating blood volume is too low or declining, high CVP suggests high intravascular volume (hypervolemia) caused by rapid or too much fluid intake (Jakobsen et al. 2010). Elevated CVP is seen in right-sided heart failure after a heart attack or high vascular resistance in the pulmonary circulation. In left sided heart failure the CVP may rise and eventually congestion can be visibly seen, with possible pulmonary oedema (Eikeland MCA. In Almaas 2010 p. 212).
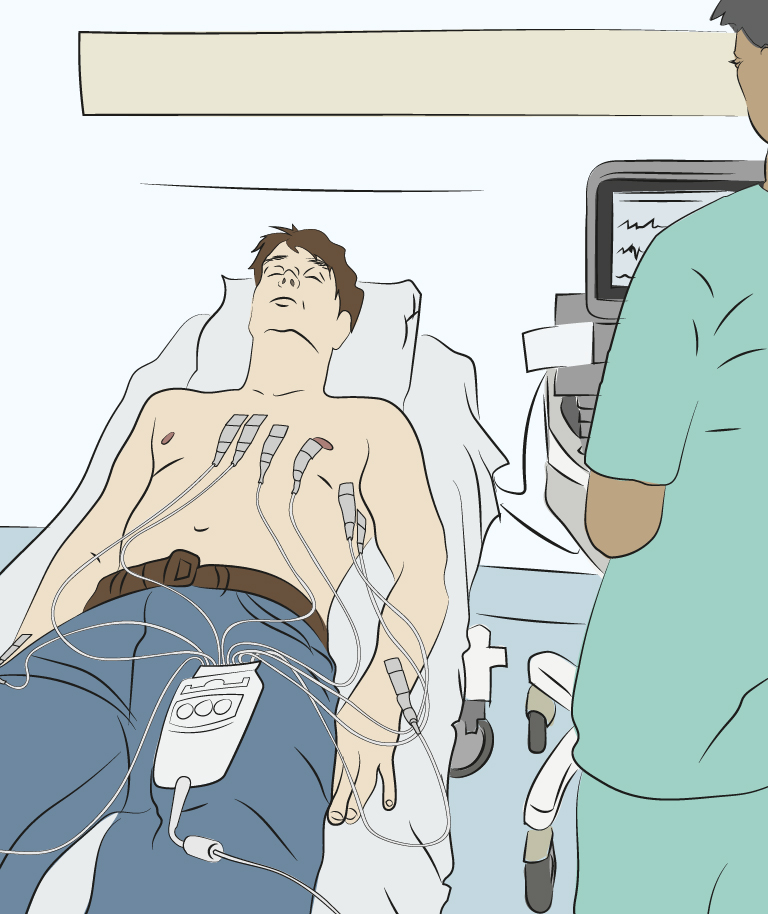
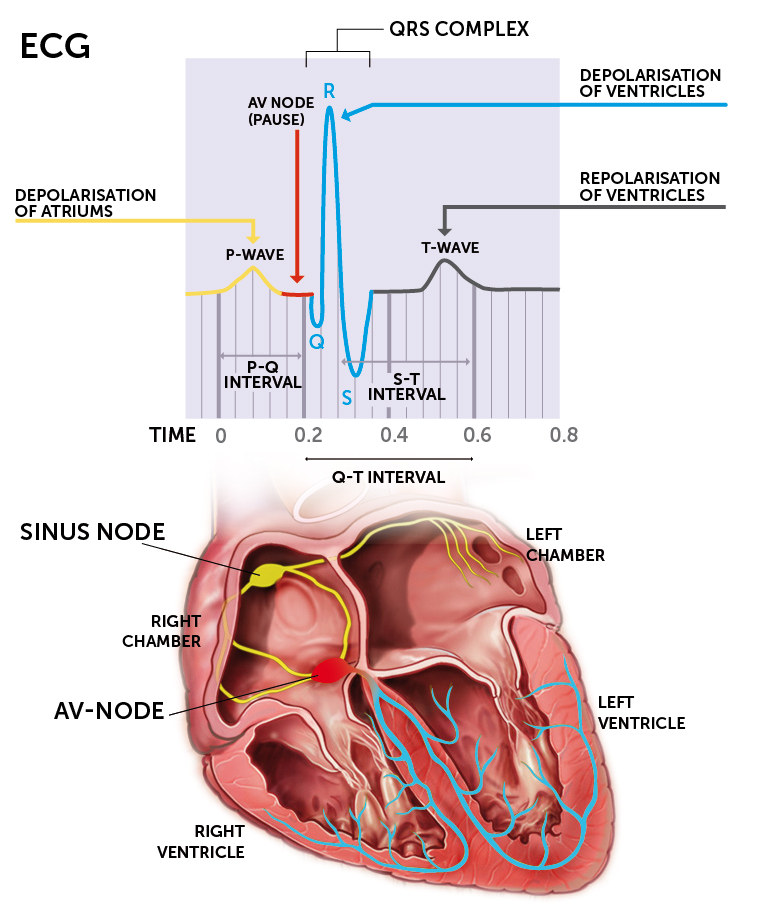
ECG (electrocardiogram) is a method for recording the heart’s electrical impulses through electrodes placed on the chest. This is an important tool to identify heart disease and to monitor the heart rhythm. The measurements performed are presented in a curve, an electrocardiogram showing the time measured in seconds. In normal ECG measurements six electrodes are placed on the chest, precordial ECG electrodes, however, for the diagnosis of ischemic heart disease a 12-lead ECG is used. The method can reveal where myocardial ischaemic damage has occurred by showing cardiac activity from different angles (Jakobsen et al. 2010).
| Exercise: Complete the sentence |
|---|